Running with an Elevated Heart Rate After COVID
As a journalist and an athlete, I like answers. And with COVID-19, there aren’t a lot of clear ones. I found this to be true after I got COVID-19 in March of 2022. I experienced lung and heart problems after COVID, including an elevated heart rate.

It was hard to find information as to why my heart rate was spiking, if it was a cause for concern, and IF I should not run until it was regulated. I found that from athletes I personally know and fellow runners in my Instagram community, having an elevated heart rate after COVID was fairly common.
Table of contents
- My Experience with Cardiac Symptoms After COVID
- FAQs about having an Elevated Heart Rate after COVID
- What the Research Finds About Cardiac Symptoms After COVID
- Why does my heart beat faster after having COVID?
- Is it normal to have a high heart rate after COVID-19?
- All of my tests came back normal, but I am still having chest pain and a rapid heart rate, what is going on?
- When should I be concerned about my elevated heart rate or heart palpitations?
- Could I have heart damage from COVID-19?
- What is the autonomic nervous system and how does COVID-19 affect it?
- How do you treat autonomic system dysfunction?
- What is Long COVID?
- Who is more at risk for long COVID and cardiac symptoms after having COVID?
- Can I start running if I am still having cardiac systems after having COVID?
But did that mean it was safe to run with a higher heart rate? I still had so many questions. So, I’ve dug into the research to share what I have learned about cardiac symptoms after COVID and long COVID to help guide you in your training and treatment.
Note: I am NOT a doctor, though this information comes from doctors and researchers. Always follow your doctor’s guidance.
My Experience with Cardiac Symptoms After COVID
I want to begin with a quick overview of what happened to me with my COVID recovery. Obviously, every case with COVID is different, which is a huge reason why it is all so confusing. But maybe, my experience can help you find answers or recover quicker.
In April of 2021, I got my second COVID shot and experienced severe chest pain later that day. I ended up in the ER with pleurisy (inflammation of the lung lining). It took me 6 weeks to recover, including a 6-week break from running. Nothing like this has ever happened to me before.
In late March of 2022, I went for a 16-mile run and felt pretty bad. I continued to feel bad the next morning. My stats on all my wearable fitness tracker, WHOOP, were all off including my Heart Rate Variability which is an indicator that you may be getting sick.
I tried to do a shake-out run and my heart rate was very high. I returned home and took a COVID-19 test which tested positive.
My Progression of COVID-19 Symptoms
I felt very sick for about 3 days including a deep cough, fatigue, and shortness of breath. A week later, I felt better and attempted to run. After four days of light running, I regressed.
I experienced heart problems after COVID including heart palpitations, heart rate spikes, chest pain, shortness of breath, and what felt like an irregular heartbeat.
I went to a walk-in clinic and got my blood drawn, a chest X-ray, and an EKG which all came back normal.
A week later, I continued to feel ill. My WHOOP kept showing my vitals out of whack including heart rate spikes. For example, when I was putting peanut butter on a bagel, my heart rate was in the 140s.
My post-COVID-19 Diagnosis & Treatment

I went to see a doctor. She diagnosed me with chest wall inflammation and sympathetic overdrive. She prescribed steroids, an inhaler, and rest.
I took a few days of complete rest and then began walking. About 10 days later, I did a 3-mile jog, alternated run days, repeated mileage, and progressed. (Read more on my return to run plan below).
My heart rate was unusually high on my runs. My resting heart rate dropped to 41 and then went up to 57 (46 is my norm). And I had brain fog and fatigue no matter how much I slept. In the third week, I felt markedly more energetic with less brain fog.
About 5 weeks into my recovery, everything began normalizing minus some chest pain and an elevated heart rate.
Why I Wrote This Article
The time scales for recovery differ for everyone. Still, I believe my COVID-19 recovery journey and research may be helpful to you.
I think while the new variants of COVID-19 may produce a milder infection, it’s important for people (especially runners) to understand it is still more taxing on the body than a bad cold and it’s important to be conservative in your return to running.
As Dr. William Li, physician, scientist, president and medical director of the Angiogenesis Foundation, and author of Eat To Beat Disease: The New Science of How Your Body Can Heal Itself, told me:
“While COVID infection has become much milder for most people, the unpredictable nature of serious aftereffects is still something the medical community is very concerned about.”
FAQs about having an Elevated Heart Rate after COVID
What the Research Finds About Cardiac Symptoms After COVID
A study, published in Nature, of more than 37,000 people recovering from COVID-19, found I was not alone in my lingering symptoms.
Tracking the data from wearables like FitBit, the researchers revealed that:
- After 9 days of first reporting symptoms, the participants’ resting heart rate dropped.
- Then, the heart rates rose and remained elevated for months. The resting heart rate was elevated 5 beats, on average.
- On average, participants had elevated heart rates for 79 days.
- Sleep and physical activity returned to baseline more slowly.
Why does my heart beat faster after having COVID?
Researchers and doctors believe the prolonged heart rate elevation is a sign that Covid-19 disrupts the autonomic nervous system,

which regulates basic physiological processes.
This explains why the heart races, palpitates and causes dizziness. This may also explain fatigue and brain fog.
“Lots of people who get Covid end up getting autonomic dysfunction and a kind of ongoing inflammation, and this may adversely affect their body’s ability to regulate their pulse,” explained one of the researchers, Dr. Jennifer Radin.
Is it normal to have a high heart rate after COVID-19?
Yes. Research shows it is normal to have a higher heart rate for more than two months after recovering from COVID-19.
In my personal experience and an unofficial Instagram poll of more than 100 runners, 85 percent had elevated heart rates. Most of these heart rates normalized in time
(Not sure when to rest, check out my article: When to Skip a Workout & How to Adjust Your Schedule)
All of my tests came back normal, but I am still having chest pain and a rapid heart rate, what is going on?
You’re in good company. Many others and I have had tests like blood tests, an EKG, x-rays, and cardiac MRIs return to normal yet still experience an elevated heart rate, shortness of breath, and chest pain.
Doctors, including my own and those at UAB, attribute this to sympathetic overdrive along with chest wall inflammation which your body should heal in time.
However, if you are concerned about your condition, consider seeing a cardiologist to get more tests and wear a Holter monitor, which monitors your heart around the clock.
“This can document when your heart rate changes, even if you cannot feel it,” explains Dr. Li.
One possible explanation for someone who develops an abnormal rise in heart rate when standing could be a condition called Postural Orthostatic Tachycardia Syndrome (POTS).
POTS is caused by an abnormality in the autonomic nervous system, which regulates blood flow back to the heart. You likely do not have POTS if your heart rate decreases each time you run or walk.
When should I be concerned about my elevated heart rate or heart palpitations?
You should be concerned about your rise in heart rate or heart palpitations, which feel like your heart is pounding, fluttering, or beating irregularly, if:
- Your heart rate does not gradually go down after exercise.
- You have chest pain.
- The occurrences are becoming more severe or more frequent, and/or
- You have a known heart condition, injury, or weak heart muscle.
- If you feel lightheaded, dizzy, or collapse during an episode of tachycardia, or elevated heart rate.
“In this case, the body is unable to compensate so the brain may not be getting enough oxygen from blood flow. This is an automatic red flag, and a signal to seek help,” warns Dr. Li, who has appeared on GMA and CNN and in The Atlantic and Time Magazine.
This is not an exhaustive list, and I am not a doctor. If you are concerned, you should go see one.
Could I have heart damage from COVID-19?
There have been fears that COVID-19 could cause myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the sack around the heart), leading to direct damage of the heart muscle.
However, this is rare.
Admittedly, when my heart rate was at the height of its irregularity accompanied by chest pain, I searched Dr. Google and was close to self-diagnosing with myocarditis as the symptoms were very similar (minus intense swelling).
However, the cause of the change in heart rate or irregular heartbeat is likely a hormonal imbalance triggered by the virus that impacts the function of the autonomic nervous system.
What is the autonomic nervous system and how does COVID-19 affect it?
The autonomic nervous system controls unconscious bodily functions such as blood pressure, heart rate, breathing rate, digestion, body temperature, and metabolism.
It is usually divided into two parts: the parasympathetic nervous system and the sympathetic nervous system.
- The parasympathetic system is often called the “rest and digest system” and controls functions that happen at rest.
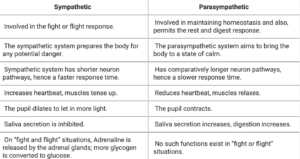
If your body perceives a threat like the COVID-19 virus, the sympathetic nervous system may overact, causing your heart to rate and breath rate to quicken.
This is what is thought to have happened to me in what my doctor called a sympathetic nervous system overdrive.
How do you treat autonomic system dysfunction?
The treatment for an imbalance of the autonomic systems varies depending on the symptoms and severity.
The treatment or way to quiet the sympathetic nervous system is often to do calming activities such as:
- gentle walks
- rest
- sleep
- deep breathing
- yoga, and
Doing something that stresses the body and elevates the heart rate such as running could worsen or elongate the COVID recovery process.
What is Long COVID?
The lingering after-effects of a COVID infection are called Long COVID and are not related to damage by the virus itself but by the body’s immune response to COVID-19.
The most common symptoms of long COVID include:
- chest pain
- heart palpitations
- abnormally high heart rates
- heart palpitations
- shortness of breath,
- and difficulty doing their normal exercise routines
Doctors theorize that long COVID and related symptoms are caused by a dysfunction of the autonomic nervous system (caused by a hormonal imbalance) thereby disrupting functions such as blood pressure, heart and breathing rates, body temperature, digestion, and metabolism.
Long COVID or long-haulers can last weeks or months and can be severe and life-altering, sadly.
Who is more at risk for long COVID and cardiac symptoms after having COVID?
Doctors say long COVID can affect anyone, even if your case is mild. It can also begin after you thought you had recovered.
There is also no evidence if anything such as exerting oneself too soon by running can contribute to long COVID.
Can I start running if I am still having cardiac systems after having COVID?
You can return to run if you still have cardiac systems after having COVID such as an elevated heart rate as long as your doctor clears you!
“If there is any lightheadedness, dizziness, or feeling of passing out — or any chest pain, shortness of breath, or palpitations, it’s time to seek out a doctor to at least make sure there is nothing serious that must be addressed. When it comes to your heart, it’s best to take no chances,” says Dr. Li.
If you do not have heart damage or a heart condition, in most cases cardiovascular exercise (for 30 minutes a day, 5 days a week) is beneficial for your COVID recovery. Get guidance from your doctor.
The key for your return to running after COVID is taking a gradual approach. For example, when you are feeling more like your normal self:
- Walk every other day for 4 days for 30 minutes. When that feels good, add a consecutive day. Then another.
- After being able to walk for 5 days for 30-60 minutes with no issue, try an easy run of 1-2 miles.
- If that feels good, begin running every other day. You can walk in between.
- After doing a run two times of a specific distance, you can add 5 minutes or a mile to your run (depending on your fitness level and how you feel).
- Continue to repeat mileage one time and alternate days.
- When you can run for an hour with no issue, try a consecutive day run.
- Be sure to keep your pace very easy—much easier than your usual easy pace.
- Continue to have at least one total rest day.
- When your mileage gets higher (like over 4 miles, don’t repeat mileage. Alternate between higher and lower mileage).
Read more about how to return to run here.
How I Returned to Running with Cardiac Symptoms After COVID:
I began a gradual return to running even though my heart rate was elevated more quickly and my resting heart rate was higher than normal. I also still had some minor chest discomfort on the right side of my chest which was diagnosed as muscular inflammation.
- I walked for about 10 days and began with a 3-mile jog. I tried another 3-mile jog two days later.
- When that felt okay, I progressed to 4 miles and so on.
- When I got to 6 miles comfortably, I tried running for consecutive days.
- Then, I progressed my mileage as normal, taking it day by day.
- I learned that keeping my easy pace about 1 minute per mile easier than my norm was key to recovering well and preventing chest pain.
What’s been your experience with COVID?





